We have all been there, neglected a niggle in our foot and told ourselves that it would probably go away. Weeks have passed, even months, and it’s only getting worse. Then finally, when we are hobbling around barely able to walk, we decide to seek help…
Well, at Achilles Foot Clinic, we are here to help you.

How Podiatrists Treat Foot Ulcers: Effective Solutions for Healing and Prevention
Foot ulcers are a common and serious concern, especially for individuals with diabetes, poor circulation, or other health conditions that affect the feet. These open sores or wounds can be painful, slow to heal, and prone to infections if not properly managed. While foot ulcers may seem like a minor issue, they can lead to severe complications, including infections, tissue damage, and even amputations if left untreated.
The good news is that podiatrists are highly skilled in diagnosing and treating foot ulcers, using a combination of wound care techniques, advanced dressings, and treatment strategies to promote healing and prevent further complications. In this blog post, we’ll take a detailed look at how podiatrists treat foot ulcers, from initial assessment to long-term prevention, and discuss the solutions that can help you heal faster and avoid future issues.
Step 1: Initial Assessment and Diagnosis
The first step in treating a foot ulcer is a thorough assessment by a podiatrist. The podiatrist will examine the ulcer, assess the surrounding skin and tissue, and determine the severity of the wound. Some of the factors they will consider include:
The size and depth of the ulcer: Deeper ulcers may require more intensive treatment.
Signs of infection: The podiatrist will check for any redness, swelling, warmth, or pus, which may indicate an infection.
Circulation and blood flow: Reduced circulation is a common cause of slow-healing ulcers, especially in individuals with diabetes. The podiatrist may check for pulses in the foot and ankle to assess circulation.
Overall foot health: Conditions like neuropathy (nerve damage), poor circulation, or deformities (e.g., bunions, hammertoes) can affect the healing process.
By evaluating these factors, the podiatrist can develop a treatment plan tailored to your specific needs, focusing on promoting healing and addressing any underlying conditions contributing to the ulcer.
Step 2: Wound Care Techniques
Proper wound care is essential for healing a foot ulcer and preventing infection. Podiatrists follow several key principles to ensure effective wound management:
Debridement:
Debridement is the process of removing dead, damaged, or infected tissue from the ulcer. By cleaning the wound and removing any necrotic tissue, podiatrists create a healthier environment for healing. There are different types of debridement techniques, including:Surgical debridement: Using specialised tools to remove tissue.
Autolytic debridement: Using dressings that help the body’s natural enzymes break down dead tissue.
Enzymatic debridement: Applying topical enzymes that dissolve necrotic tissue.
Debridement promotes faster healing by ensuring that healthy tissue can regenerate.
Infection Control:
If an infection is present, the podiatrist will clean the ulcer thoroughly, using antiseptic solutions to kill bacteria. In some cases, antibiotics may be prescribed to treat an infection. Keeping the ulcer clean is essential to prevent further complications, such as cellulitis or bone infections (osteomyelitis).Moisture Balance:
The environment of the wound plays a significant role in healing. Wounds that are too dry or too wet can both impair the healing process. Podiatrists use advanced dressings to maintain an optimal moisture balance, creating a protective barrier over the wound while promoting the body’s natural healing process.
Step 3: Advanced Dressings for Optimal Healing
The type of dressing applied to a foot ulcer is a critical aspect of the treatment process. Podiatrists choose dressings based on the size, depth, and condition of the ulcer. Some of the most commonly used dressings include:
Hydrocolloid Dressings:
These dressings form a gel-like substance when they come into contact with wound exudate, maintaining a moist environment that promotes faster healing. Hydrocolloid dressings are particularly effective for ulcers with moderate exudate.Foam Dressings:
Foam dressings are highly absorbent and are often used for wounds with heavy drainage. These dressings help maintain moisture while also preventing the wound from becoming too wet, which can lead to further tissue damage.Alginate Dressings:
Made from seaweed, these dressings are highly absorbent and ideal for ulcers with significant drainage. They help control infection and support wound healing.Antimicrobial Dressings:
For infected ulcers, antimicrobial dressings containing silver or iodine can be used to reduce the risk of bacterial growth and infection.Biologic Dressings:
In some cases, podiatrists may use biologic dressings, which are made from human, animal, or synthetic materials. These advanced dressings can support tissue regeneration and promote healing in more severe cases.
By choosing the right type of dressing, podiatrists can enhance the healing process, reduce the risk of infection, and provide comfort to patients during recovery.
Step 4: Pressure Offloading
For ulcers caused by pressure, particularly those on the bottom of the feet, pressure offloading is crucial for effective healing. This involves relieving the pressure on the affected area to prevent further injury and promote healing. Some techniques include:
Specialised footwear: Podiatrists may recommend custom-made shoes or insoles that reduce pressure on the ulcer while providing cushioning and support.
Total contact casting: In severe cases, a podiatrist may use a special cast to immobilise the foot and protect the ulcer from pressure. This is especially common for diabetic ulcers that occur on the bottom of the foot.
Walking aids: Crutches, a cane, or a walker may be used to help reduce weight-bearing on the ulcer while it heals.
Offloading the pressure on the affected area is essential for preventing further damage and giving the ulcer a chance to heal.
Step 5: Monitoring and Follow-up Care
Once the ulcer has been treated, regular follow-up appointments are essential to ensure that the wound is healing properly. During these visits, the podiatrist will:
Assess the progress of the healing process.
Check for signs of infection or complications.
Adjust dressings or treatment plans as needed based on the ulcer’s condition.
Ongoing care and monitoring help ensure that the ulcer heals properly, and that complications are avoided.
Preventing Future Foot Ulcers
Prevention is always better than treatment, and for those at risk of foot ulcers, it’s essential to take steps to reduce the likelihood of developing them in the first place. Some preventive measures include:
Daily foot inspections: Regularly check your feet for cuts, blisters, redness, or swelling, especially if you have diabetes.
Proper footwear: Choose shoes that fit well, offer support, and reduce pressure on your feet.
Moisturise: Keep your feet hydrated to prevent dry, cracked skin that could lead to ulcers.
Blood sugar management: For diabetic patients, maintaining healthy blood sugar levels can help prevent nerve damage and circulation issues, both of which contribute to foot ulcers.
Conclusion
Foot ulcers are a serious condition that requires careful attention and treatment. Podiatrists play a crucial role in not only healing existing ulcers, but also in preventing new ones from forming. By utilising advanced wound care techniques, effective dressings, and strategies like pressure offloading, podiatrists can help patients heal faster and avoid severe complications.
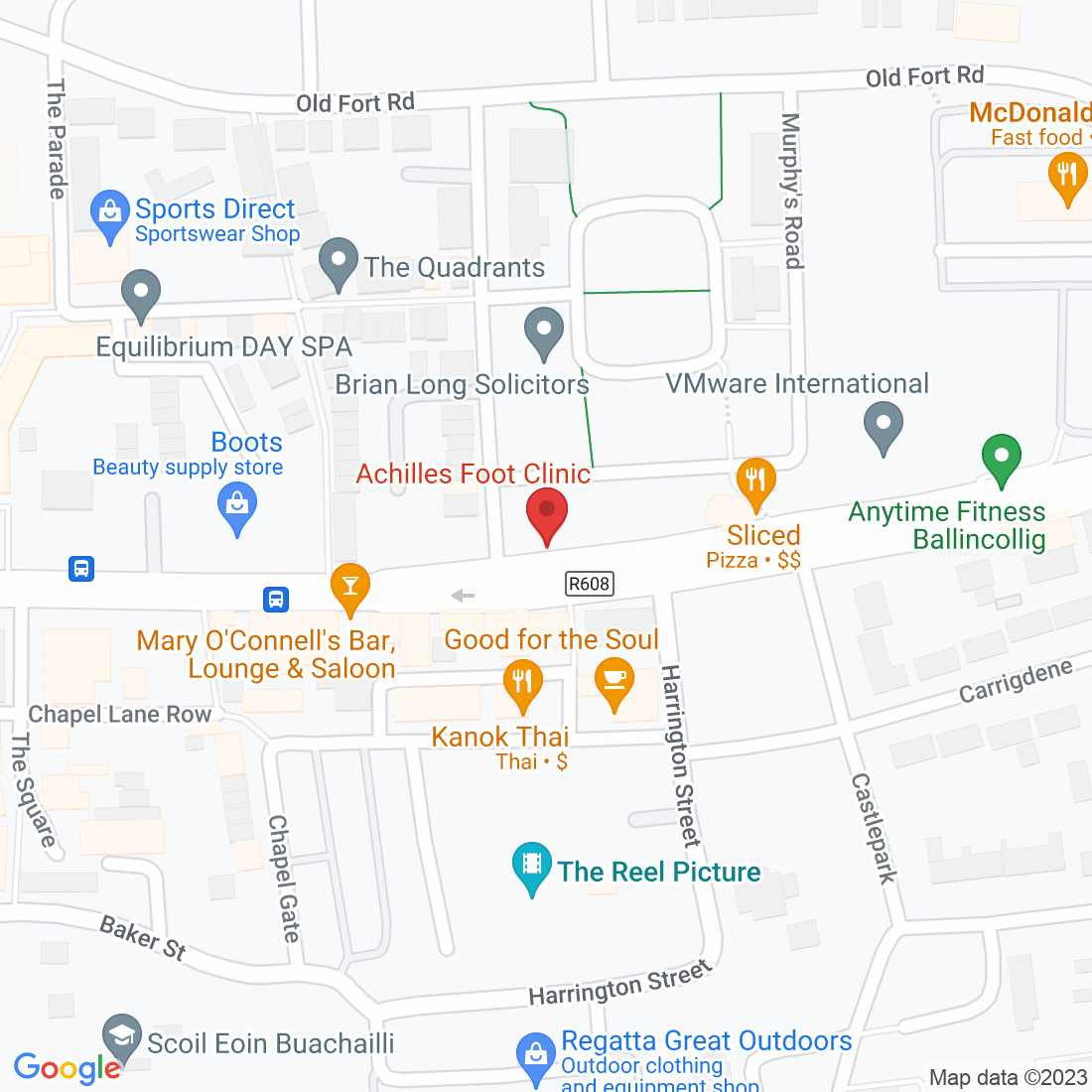
If you are dealing with a foot ulcer or are concerned about foot health, don’t hesitate to reach out to Achilles Foot Clinic. Our expert podiatrists are here to help you with tailored solutions to promote healing, prevent further issues, and keep your feet healthy.
Contact us today to schedule an appointment and start your journey to healthy, pain-free feet!
Ask Lorcan And His Team
Fill in the form to request a Call From Our Team
Fill in the form to request a Call From Our Team
One of our team will call you for FREE and answer any questions or concerns you may have about Bunions.
One of our team will call you for FREE and answer any questions or concerns you may have about your uncomfortable Bunions.