We have all been there, neglected a niggle in our foot and told ourselves that it would probably go away. Weeks have passed, even months, and it’s only getting worse. Then finally, when we are hobbling around barely able to walk, we decide to seek help…
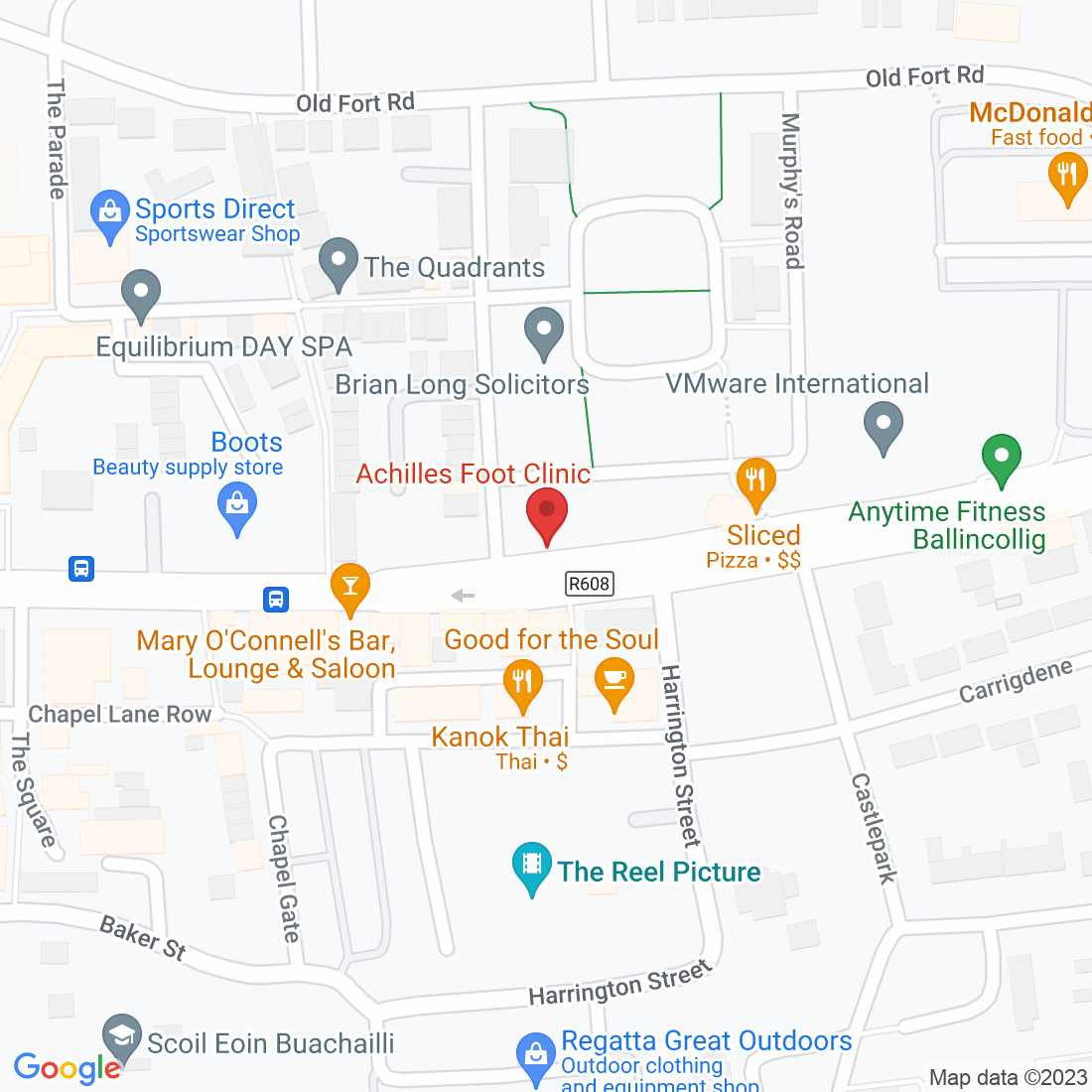
Well, at Achilles Foot Clinic, we are here to help you.

The Connection Between Athlete’s Foot and Toenail Fungal Infections: Diagnosis and Treatment
At Achilles Foot Clinic, we often see patients struggling with fungal infections affecting both their feet and toenails. Two common issues that frequently appear together are athlete’s foot and toenail fungal infections. Understanding their connection can be crucial for effective diagnosis and treatment. In this blog post, we’ll explore how these conditions are related, how they can be diagnosed, and the best approaches for treating them.
Understanding Athlete’s Foot and Toenail Fungal Infections
Athlete’s Foot (Tinea Pedis): This is a fungal infection that affects the skin on the feet, often between the toes. It's caused by dermatophytes, a type of fungus that thrives in warm, moist environments like public showers or swimming pools. Symptoms include itching, burning, and peeling of the skin.
Toenail Fungus (Onychomycosis): This infection affects the toenails, causing them to become discoloured, thickened, and brittle. It is also caused by dermatophytes, but in some cases, yeast or moulds can be involved. Toenail fungus can start from an athlete’s foot infection or occur independently.
The Connection Between Athlete’s Foot and Toenail Fungus
Shared Fungal Pathogens: Both athlete’s foot and toenail fungus are caused by similar types of fungi. If the fungi causing athlete’s foot are not treated promptly, they can spread to the toenails, leading to a more severe and persistent infection.
Common Risk Factors: Factors such as excessive moisture, tight-fitting shoes, and poor foot hygiene can contribute to both conditions. Athletes or individuals with sweaty feet who frequently wear closed shoes are at higher risk of developing both athlete’s foot and toenail fungus.
Potential for Spread: Athlete’s foot can serve as a gateway for fungal infections to enter the toenails. The same fungal pathogens can move from the skin to the nails, exacerbating the infection.
Diagnosing Combined Infections
Accurate diagnosis is key to effective treatment. Here’s how healthcare professionals typically approach diagnosing these conditions:
Clinical Examination: A thorough physical examination is the first step. The doctor will look for signs of athlete’s foot such as redness, peeling, or itching, and inspect the toenails for discolouration, thickening, or crumbling.
Microscopic Examination: A skin scraping or nail clipping may be taken and examined under a microscope to identify the presence of fungal elements.
Fungal Cultures: Culturing samples from the affected skin or nails can confirm the type of fungus causing the infection, which helps tailor the treatment approach.
Dermatological Tests: In some cases, additional tests like a KOH (potassium hydroxide) preparation or biopsy may be conducted to rule out other conditions and confirm fungal infections.
Treatment Approaches for Combined Infections
Treating athlete’s foot and toenail fungus often involves addressing both conditions simultaneously. Here’s a comprehensive approach to managing these infections:
Topical Antifungal Treatments:
For Athlete’s Foot: Over-the-counter antifungal creams, powders, or sprays can be effective. These products are applied directly to the affected skin and help eliminate the fungus.
For Toenail Fungus: Topical antifungal nail lacquers or creams can be prescribed, though they may be less effective for severe infections.
Oral Antifungal Medications:
Oral antifungal drugs like terbinafine or itraconazole are often prescribed for toenail fungus, especially when topical treatments fail. These medications work systemically to eliminate the fungus from within the nail.
Proper Foot Hygiene:
Keeping feet clean and dry is crucial. Wash your feet daily, dry them thoroughly, and use antifungal powders or sprays if recommended. Avoid walking barefoot in public areas and wear moisture-wicking socks.
Nail Care:
Regularly trim and thin affected toenails to reduce fungal load. In severe cases, partial or complete removal of the infected nail may be necessary to allow effective treatment.
Environmental Measures:
Disinfect shoes, socks, and other items that come into contact with the feet. Fungal spores can persist on surfaces and reinfect the feet.
Follow-Up and Prevention:
Regular follow-up with your podiatrist is essential to monitor progress and prevent recurrence. Preventative measures include wearing breathable footwear, maintaining good foot hygiene, and avoiding sharing personal items.
Conclusion
The connection between athlete’s foot and toenail fungal infections highlights the importance of comprehensive treatment and management. By understanding how these conditions relate and adopting effective diagnostic and treatment strategies, you can address both infections and work towards complete resolution.
If you’re dealing with athlete’s foot or toenail fungus, or if you have any concerns about your foot health, don’t hesitate to contact Achilles Foot Clinic. Our team of experts is here to provide personalized care and help you achieve healthy, fungus-free feet.
Contact us today to schedule a consultation and learn more about effective treatments for fungal infections.
Ask Lorcan And His Team
Fill in the form to request a Call From Our Team
Fill in the form to request a Call From Our Team
One of our team will call you for FREE and answer any questions or concerns you may have about Bunions.
One of our team will call you for FREE and answer any questions or concerns you may have about your uncomfortable Bunions.